Study population
This study was conducted at the sleep clinic of Seoul National University Bundang Hospital (SNUBH), Seongnam, Korea. Healthy adults, aged 20–65 years, were recruited by advertisements in the local community from August 2020 to August 2021. The enrolled participants underwent screening tests at the first visit, which was within a week prior to the initiation of intervention. Those who experienced adverse skin reactions in the screening test were excluded. We also excluded those who met the following criteria: (1) history of light therapy or vitamin D supplementation within two months prior to study entry; (2) skin diseases including skin cancers and photosensitivity; (3) medical illnesses such as malignancy, respiratory diseases, infectious diseases, hepatic or renal impairment, and head trauma; and (4) psychiatric disorders including mood disorders, anxiety disorders, sleep disorders, and psychotic disorders. Written informed consent was obtained from all participants before the initiation of the study. This study was approved by the Institutional Review Board of SNUBH (B-2002-597-003) and was registered with the Clinical Research Information Service (CRIS), Republic of Korea (registration number KCT0007033).
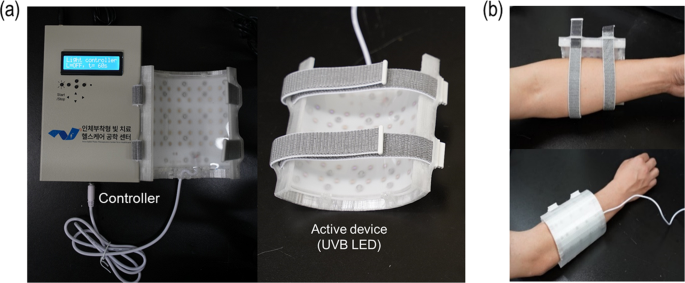
Intervention
We used two different types of proto-type wearable light-emitting devices (the active and sham device), which were custom-designed at the School of Electrical Engineering, Korea Advanced Institute of Science and Technology, Daejeon, Republic of Korea. The active device was composed of 48 LEDs (QD Jason, China, Model J35ABA285P09A) that emitted UVB light at a peak wavelength of 285 nm with the full width at a half-maxima of 11 nm. LEDs were arranged on a flexible printed circuit board (FPCB) in a 6 × 8 matrix format with an interval of 13 mm between adjacent LEDs. Then, the FPCB with these 48 UVB LEDs was placed in a 3-D printed housing that could be wrapped around the lower or upper arm. The distance between an LED and the surface of the skin under illumination was maintained at ~5 mm to ensure that light from the LEDs could spread over the skin. Furthermore, a clear elastomer of polydimethylsiloxane (PDMS) was placed between the LEDs and the surface of the skin to ensure that the skin-to-LED distance remained constant. One side of the PDMS layer was micro-structured to further enhance the spread of the LED light. The overall illuminated area was ~80 cm2. The light-diffusing structure could sustain a dose of ~7.8 mJ/cm2 per one-min exposure. The sham devices had an identical construction except that the LEDs emitted blue light with a peak wavelength of 465 nm instead of UVB light (Fig. 1).
At the first visit, a screening test was conducted using a testing device made of a single LED, which emitted UVB light with the same wavelength and intensity as the active device, onto a 3-cm2 area of forearm skin. Thereafter, the eligible participants were randomly assigned at a 1:1 ratio to either the experimental or control group and were blinded to the intervention assignment. The random assignment was performed by a third party, via the stratified permuted block randomization method. At the second visit, which was within a week after the first visit, the participants received either the active or sham device depending upon their randomized group assignment. They were instructed to wear the device for a total of 2 min, 1 min on each forearm every day for 4 weeks. One minute of UV exposure on each arm was controlled by the controller unit of the devices. Accordingly, the daily dose per unit area of UVB radiation by the active device was determined as approximately 7.8 mJ/cm2, and the effective area of exposure was ~80 cm2 for each forearm, making the total daily dose of 1.25 J (=7.8 mJ/cm2 × 80 cm2 × 2). For the safety of the participants, we monitored the occurrence of any adverse events and compliance with device use at the third and four visits, which took place 2 and 4 weeks after the initiation of the intervention, respectively. If any suspicious adverse skin reactions including erythema or rash occurred after the intervention, the use of the device was immediately discontinued, and the participant was withdrawn from the trial.
Serum 25-hydroxyvitamin D measurement
We adopted serum 25-hydroxyvitamin D [25(OH)D] concentrations as the indicator of serum vitamin D nutritional status since it is widely used for the measurement of serum vitamin D nutritional status [17]. Serum 25(OH)D concentrations were measured using a high-performance liquid-chromatography-tandem-mass-spectrometry method. Vitamin D is metabolized through the liver and kidneys and its metabolism is related to serum calcium and phosphate [18]. Therefore, the serum levels of calcium, phosphate, alanine transaminase, aspartate aminotransferase, alkaline phosphatase, gamma-glutamyl transpeptidase, total bilirubin, creatinine, and blood urea nitrogen were also assessed simultaneously with the serum 25(OH)D measurements. Blood tests were conducted four times, at the first (baseline), third (week 2), fourth (week 4), and final visits. The final visit was conducted two weeks after the end of the intervention (week 6). All the blood samples were collected during the daytime (from 9:30 A.M. to 4:00 P.M.), in the non-fasting state, and were properly processed and transported to the testing institute (Seoul Clinical Laboratories, Seoul, Republic of Korea). All the blood tests were performed at the same time of the day for each participant. In addition, the season during which the participants were enrolled in the study was considered as a confounding factor due to seasonal variation of serum 25(OH)D levels in Korean adult population [19]. Our study participants were categorized into four groups according to the season of study enrollment: spring (March to May), summer (June to August), autumn (September to November), and winter (December to February) group.
Demographic characteristics
Demographic information, including age, sex, body mass index, marital status, education level, current smoking status, drinking habits, and physical activity level, was obtained at the first visit. As for drinking habits, the participants were grouped as positive if they had consumed any alcohol at least once in the past month. With regard to the physical activity level, those who performed any kind of exercise for at least 30 min each, three times a week were classified as positive.
Nutrition and outdoor activities
Serum 25(OH)D levels can be affected by the skin production of vitamin D via sunlight exposure or dietary supplementation. Therefore, we examined the daily amount of dietary vitamin D intake and time spent on any outdoor activities at 2 and 4 weeks of intervention and 2 weeks after the end of the intervention. All participants were instructed to keep a daily diary of their diet and outdoor activity levels during the entire 4 weeks of the intervention period and the additional 2 weeks after the end of the intervention. We also calculated the average daily amount of dietary vitamin D intake and time spent on outdoor activities from the start of intervention to each assessment.
Statistical analysis
We calculated the minimal required sample size as 128 subjects (64 for each group), using G*Power software at a confidence level of 95%, an effect size of 0.5, and statistical power of 0.8. Effect size of 0.5 was adopted as it represents “medium” effect size. Considering the drop-out rate of 15%, we decided to enroll no fewer than 150 subjects (75 in each group). In the current study, a per-protocol (PP) analysis was performed after excluding the data from those who had dropped out.
Baseline demographic characteristics were compared using the independent t-test or Mann Whitney U test for continuous variables and the chi-squared test for categorical variables between the experimental and control groups. With regard to changes from baseline at each serum 25(OH)D level assessment, paired t-test and independent t-test (or Mann Whitney U test) were adopted to evaluate intra-group differences and inter-group differences, respectively. An analysis of covariance was also conducted to compare the changes in serum 25(OH)D levels after controlling for possible confounding factors. As a sub-analysis of the experimental group, we used independent t-test and ANCOVA to compare the changes of serum 25(OH)D levels after 4 weeks of intervention between those with and without vitamin D deficiency at the baseline assessment. Vitamin D deficiency was defined as serum 25(OH)D levels <20 ng/ml [20]. All statistical analyses were performed using SPSS version 25.0 for Windows (SPSS, Chicago, IL, USA) and a two-tailed p value of less than 0.05 was considered statistically significant.